Access QI Collaborative Learning Session 1: Understanding your system
The Access QI collaborative is a partnership between Healthcare Improvement Scotland (HIS) and NHS Education for Scotland (NES), with support from the national Centre for Sustainable Delivery (CfSD). The collaborative is currently helping Gynaecology, Urology, Ear, Nose and Throat (ENT) and other elective care services across Scotland use quality improvement (QI) methods to sustainably and affordably improve waiting times.
To begin the improvement journey, the elective care teams and colleagues from HIS, NES and CfSD all came together in September 2022 for their first learning session at The Studio in Glasgow. Through a combination of teaching and hands-on group activities, the teams learned how to use service data and QI tools to understand their systems, identify system constraints, and decide where to focus their improvement efforts.
A Call to Action from our Director of Improvement
The day began with a few inspiring words from Ruth Glassborow, Director of Improvement for HIS. She opened by acknowledging the many system pressures currently faced by NHS services, as well as the inherent challenges of finding time for service improvement work.
Ruth then remarked that in any crisis there is nevertheless an opportunity, and that under the current pressures, teams will only exhaust themselves if they keep doing things in the same way: “The reality is that we need to do some things radically differently and go down the road less travelled.” To illustrate the value of putting the time and effort into improvement work, she highlighted examples of NHS teams who have made impactful changes. A mental health team in NHS Borders streamlined their pathway by mapping their processes and eliminating unnecessary steps. A hysteroscopy pathway in NHS Tayside reduced average wait times from 137 days to just 34 days by instituting a one-stop clinic.
Ruth then explained that to achieve this kind of impact, it’s crucial to understand your system first, then focus your efforts on the areas that matter most: “This kind of work delivers because people took the time to understand their pathways, to do process mapping, to talk to people using the services, to talk to staff about what could be done more efficiently.” She concluded by encouraging the teams to look forward to the sense of empowerment that comes from choosing to make meaningful changes.
“We’re living in a world where we feel like change is imposed upon us, things are done to us, which is more stressful. When you choose to change, when it’s your choice as an individual or a team, it becomes more enjoyable, and when you see the impact of those changes, it is really inspiring.” – Ruth Glassborow, Director of Improvement for Healthcare Improvement Scotland
Systems and the theory of constraints
The teams were led through a session on systems, system constraints, and the use of data to locate and remedy constraints. To kick things off, they first learned about the theory of constraints. The theory proposes that a bottleneck or constraint within a system determines the pace of the whole system, and suggests a 5-step framework to address the constraint. To get the attendees to think about this further, they divided into groups of five and played a waiting list game to demonstrate the theory of constraints in practice.
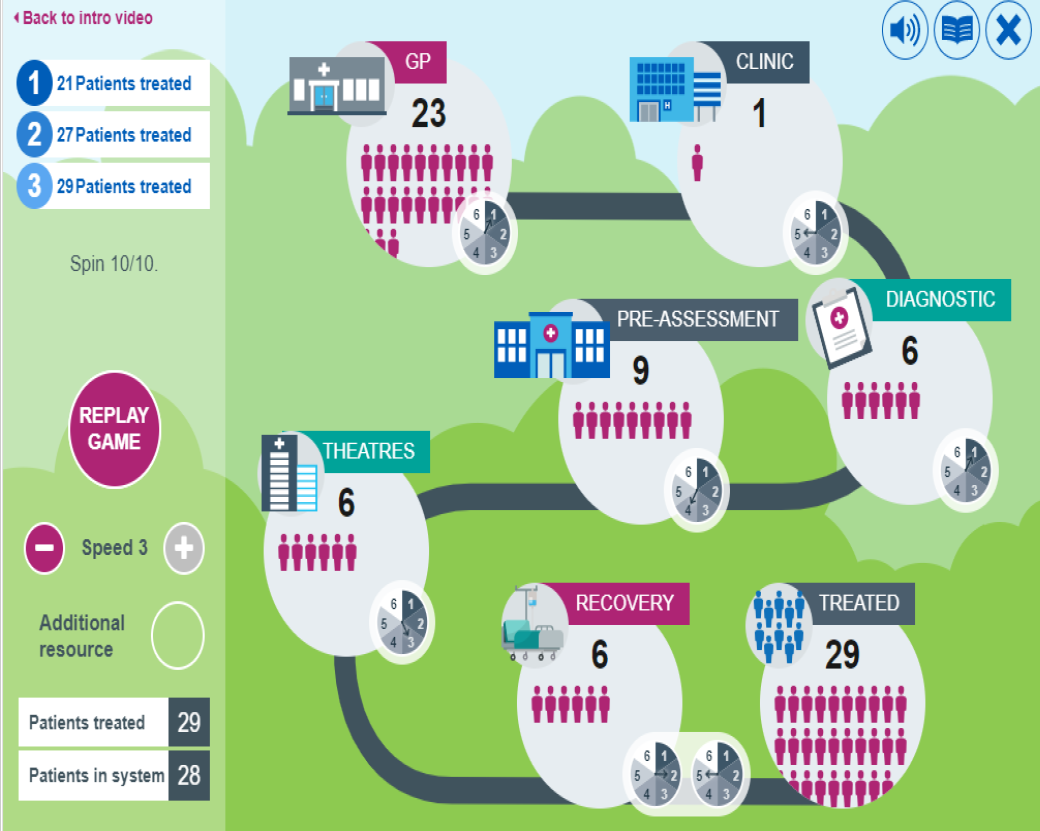
An image showing the simplified patient pathway used in the waiting list game
The game represents a simplified version of a patient pathway, with each group member representing a different stage in the pathway: GP, Outpatients, Diagnostics, Treatment, and Discharge. They took turns rolling dice to determine the capacity to see patients at each stage. The goal is to get as many patients from the start of the pathway to the end, without a backlog of patients in any one part of the system. In the first version of the game, the teams had no additional resources. In the second, they were allowed to choose one part of the pathway to give an additional resource. In the third version, they could move the additional resource wherever they wanted in between rounds.
After completing the three scenarios of the game, each group was asked to reflect on the experience. One group remarked on the “satisfaction of having some control over where you were putting the resource rather than having it stuck in one place,” in the third version. Another group echoed this sentiment, saying, “The idea about flexibility and giving people on the ground control, that made the difference.” This last round of the game allowed them to look at the number of patients waiting at each stage, and then make a decision based on what that data was telling them.
Digging into Demand, Capacity, Activity and Queue
The waiting list activity led into a discussion of Demand, Capacity, Activity and Queue (DCAQ), and how these elements can show you what is happening within your system.
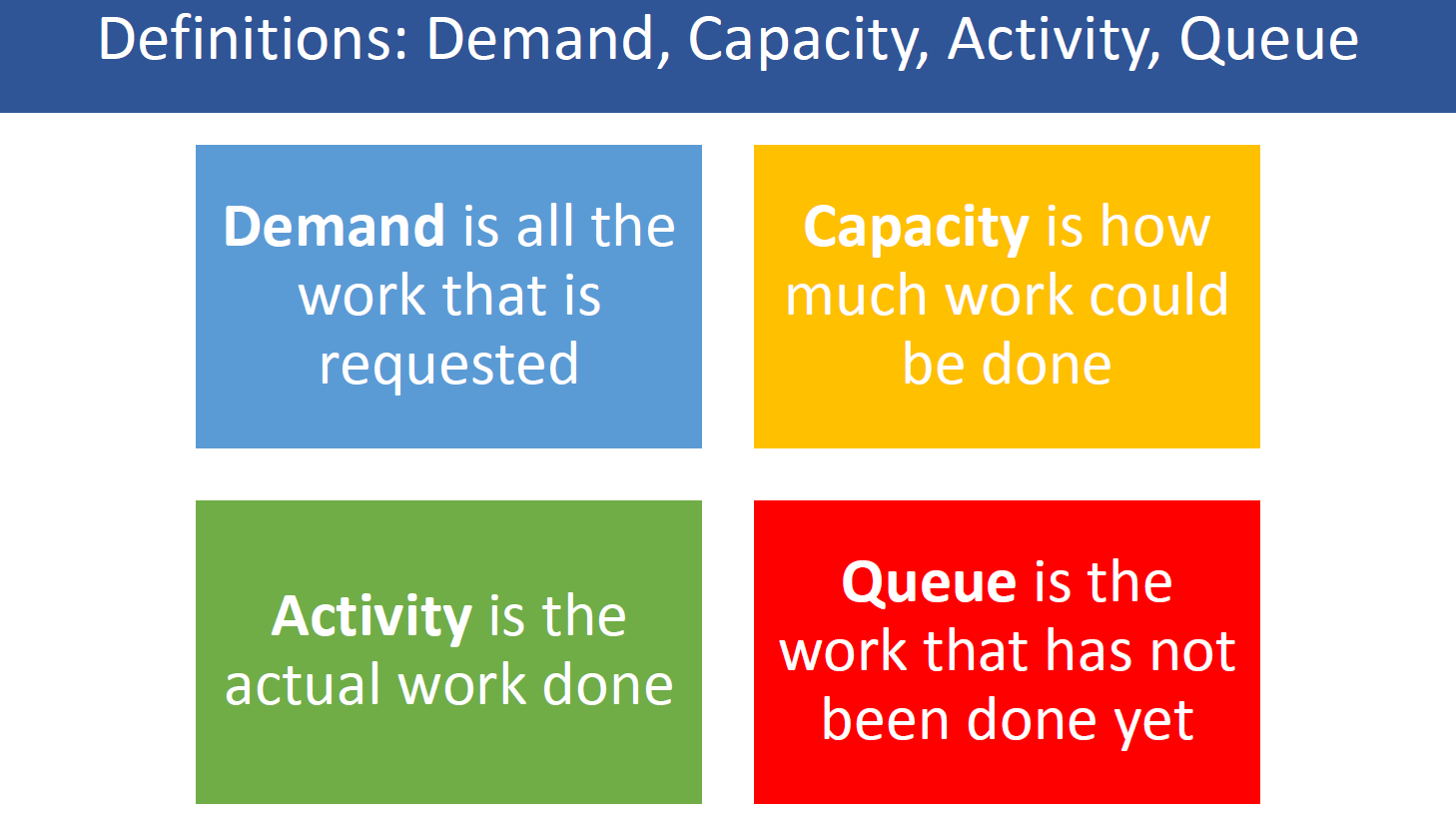
A diagram defining each element of DCAQ
The interaction of demand, capacity, and activity all impact the queue, so it’s important to balance them for a sustainable system. Each team then gathered together to look at their own service data and discuss what the data told them about DCAQ. The teams all noticed different things about their services:
- One team looked at variations in demand before, during, and after the COVID-19 pandemic in hopes of understanding what caused the variation.
- Another team reflected that there were so many layers of things happening in their system that they would need to decide what to prioritise and then look at that area in more detail.
- A third team found it interesting to look at a high level view of referrals coming into the service, particularly at the large number of routine referrals.
Specialty breakout discussions
To allow the groups to learn from each other and exchange ideas about where they might focus their improvement efforts, the larger group was then split up by specialty with members of the Access QI team helping lead the discussions.
- In the Gynaecology group, it was discovered that many of the teams plan to work on their postmenopausal bleeding pathway, so can hopefully share their learning with each other along the way. They talked about the realities of keeping up with growing waiting lists and the potential impact of working with primary care to tweak referral processes.
- In the ENT group, teams discussed the challenges of working within such a varied specialty and trying to ensure that each patient is referred to the right person at the right time. One team shared their experience of developing a data dashboard, which has helped them track waiting lists and adjust appointment availability accordingly. They will hopefully share more about this with the other teams in the coming months.
- In the Urology group, a team shared that they planned to focus on diagnostics and spoke about some of the challenges of obtaining in-depth data about their service.
Mapping patient pathways
After a break for lunch, the groups moved on to a session about process mapping. A process map visually describes the flow of work through a system. It should include the beginning and end of the process, each step taken, and points where decisions are made. It shows what is actually happening in a system, not what you think is happening or should be happening, and therefore can be extremely useful in identifying system constraints. The teams were encouraged to consider each step of the pathway they wish to improve, as well as the time spent at and between steps, and the patient experience throughout.
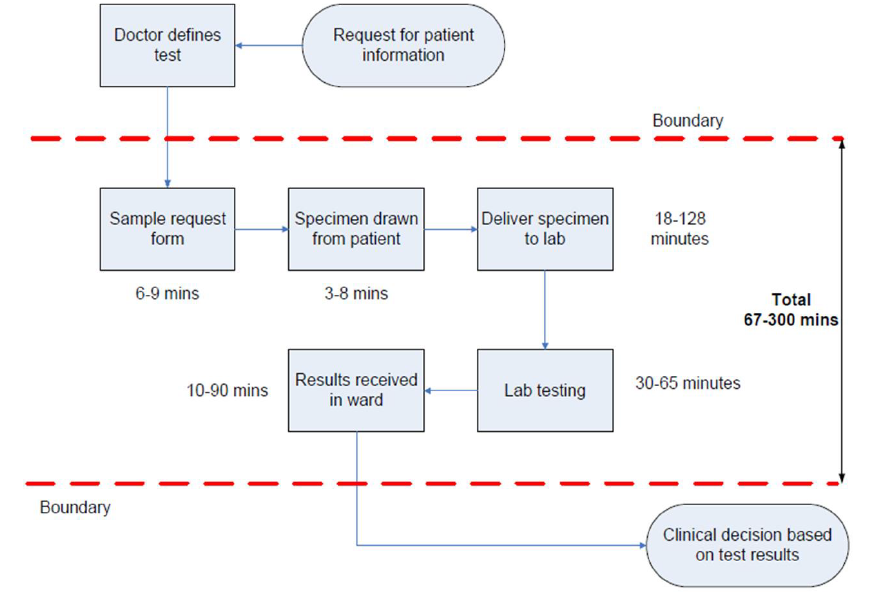
An example of a process map
The teams then got straight to work creating their own process maps on large sheets of paper. They began with high level steps, like referral from GP, appointment with outpatients department, and treatment. Next, they considered more detailed steps, like a secretary allocating appointment slots for the week or sending out appointment letters. Each team took their own unique approach. Some groups wrote their steps on sticky notes and then arranged them into the correct order. One team tentatively wrote steps in pencil, then went back and finalised them with markers once they had agreed on each step. The room was bustling with conversation as the teams mulled over their pathways and deliberated how to visualise them.
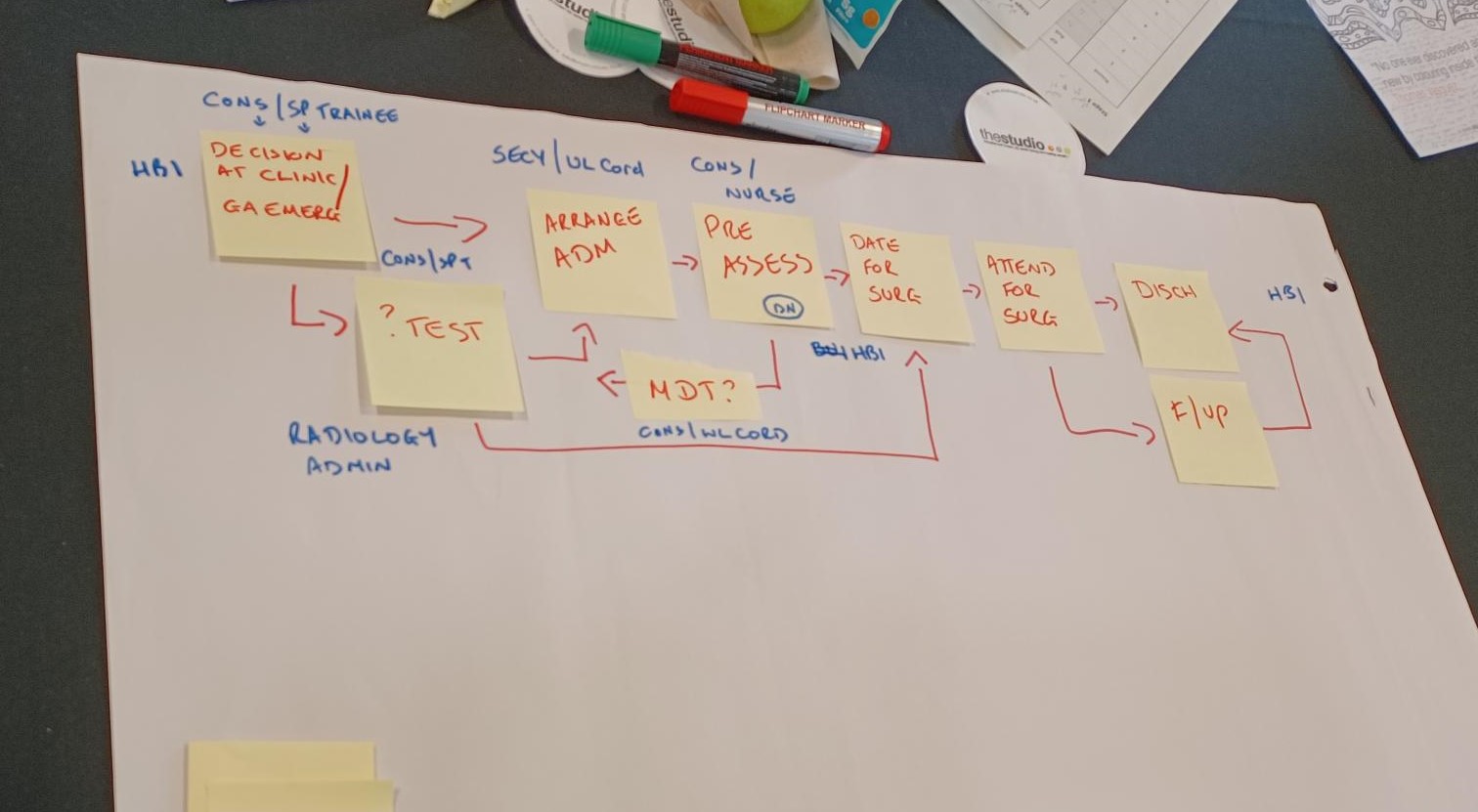
A team’s process map in progress
“We enjoyed the opportunity to put this down. It’s important to set out the starting point and really look at the work as it is done – there was no room for ‘should’ at the table.” – Participant from NHS Tayside
What comes next?
After process mapping, some participants remarked that mapping helped them look at where to focus their efforts, while others noted that they didn’t feel they had enough data yet. The NES facilitators suggested that as a next step, the teams could ‘drill down’ further into one or more elements of DCAQ to see what’s contributing to them. They were also encouraged to contemplate how they might resolve DCAQ issues by reducing demand or maximising their capacity. The Access QI: Improving planned care pathways toolkit is brimming with tools and resources that will help teams achieve all of this in the coming weeks and months of the Access QI Collaborative.
The day concluded with an opportunity for teams to devise an action plan, or a list of actions to carry out based on their learning from the day. This might include obtaining more data, taking more time to interpret the data they already have, or spending additional time on process mapping.
“The more we understand our data and the more we understand the reasons behind it, that can really inform the improvements we want to make.” - Julia Mackel, Principal Lead for NES
After a productive day the session wrapped up with a big thank you to the teams for their hard work and reminder of upcoming project surgeries, which will allow them to give project updates and ask any questions they might have. The Access QI teams will all reconvene virtually on 16 November for Learning Session Two, which will focus on understanding the system from the viewpoint of people who use services.


